What do we mean by integrated working
In any discussion of integrated working, a first prerequisite is that all parties define what they are talking about. Integrated working is one of those terms that has come to mean different things to different people so it is essential to ensure that everyone is talking about the same thing. A review by Hilary Robertson for the Royal College of Nursing in Scotland (Robertson, 2011) quotes a paper identifying 175 different definitions related to integration.
The word cloud below (drawing on Leathard, 2003) illustrates just some of the terms that can be associated with any discussion of integrated working.

Learning outcomes
- Identifying the different definitions and interpretations that are put on integrated working
Time
- No more than 30 minutes
Materials
- Post-its (using different colours for different professional groups is useful), flip chart, copy of word cloud
Guidance
- Divide into groups of four or five.
- Each individual to write words or phrases which indicate their understanding of integrated working on post-its, one to each post-it [5-10 mins]; a leader in each group to go round the group getting a word (and post-it) from each individual in turn until all the ideas are exhausted. As the post-its are handed over group them into themes.
- Discuss similarities and differences across the definitions and identify whether there are differences or similarities across different professional groups.
- Show a copy of the word cloud above, confirming the wide range of terms that can be used – Leathard characterises it as a ‘terminological quagmire’.
- Suggest that a useful way forward is to focus on the individual and to think of the delivery of integrated care and support to that individual such that the individual experiences seamless provision. Integrated working can then be seen as the route to the achievement of this integrated care and support.
A key distinction which should be drawn is between integrated structures and integrated care and support. It is useful to focus on the individual and to think of the delivery of integrated care and support to that individual. Integrated working can then be seen as the route to the achievement of this integrated care. It is also helpful to think of integrated working as taking place at different points along a continuum from autonomy through co-ordination to structural integration. This is represented diagrammatically below (NHS Confederation, 2010).
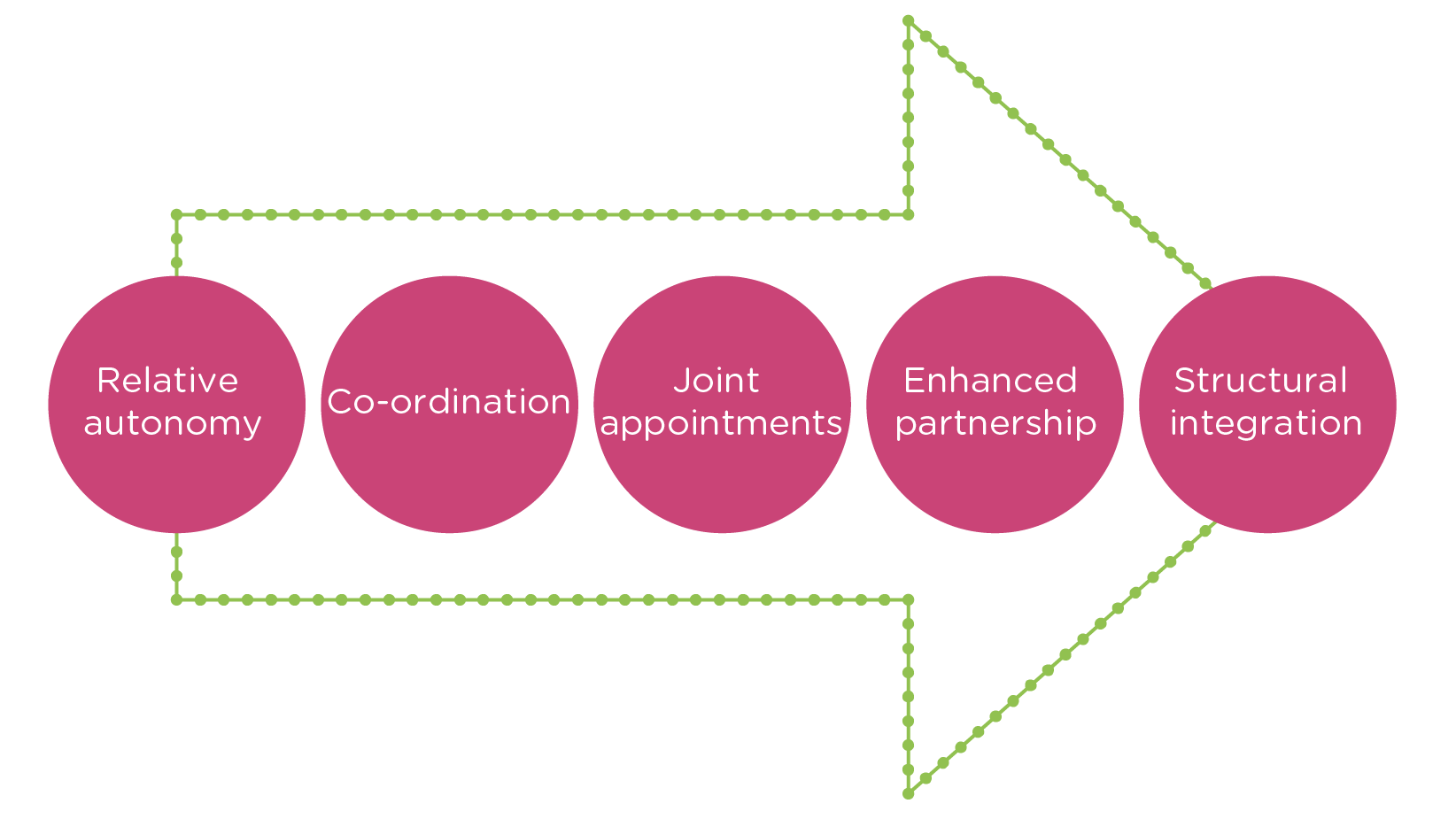
The definitions associated with this continuum relate in this context to health and social care but are relevant to other partnership arrangements also.
- Relative autonomy: the local authority and NHS meet statutory requirements for formal partnership working, but most co-ordination is largely informal
- Co-ordination: there is a reasonable level of formal commitment to joint working, with co-ordination around some areas of strategy and/ or commissioning depending on circumstances
- Joint appointments: health and the local authority have some key joint appointments and the teams collaborate but are not integrated/combined
- Enhanced partnership: a system-wide commitment, shared vision and integration across most strategic and commissioning functions, senior and middle-tier joint appointments, formal high-level backing, but separate entities remain
- Structural integration: health and local authority care services have formed a single integrated legal entity or a combined service
Particularly important for the current context is to clarify the level at which integrated working is being discussed. This can be at the individual level – different professions working together; at the organisational level – different organisations seeking to deliver a seamless service; and at the structural level – strategic planning. The primary focus for this guide is the delivery of outcome-focused practice either in integrated teams or where individuals from different professions are seeking to work together to deliver integrated care and support.
Glasby et al (2011) use the idea of breadth versus depth to characterise the relationships that signify integrated working. Breadth refers to the number of agencies (or alternatively different professional groups) that are involved in the relationship; depth is similar to the continuum highlighted above and indicates the nature of the activities included within the relationship.

from Glasby et al (2011)
Policy context
There is a lengthy history of moves towards partnership working and greater integration in Scotland. Successive health White Papers in 1997 (Designed to Care) and 2003 (Partnership for Care) promoted a partnership agenda. The former established Local Health Care Co-operatives (LHCCs), replaced in turn through the latter by the establishment from April 2005 of Community Health (and Care) Partnerships.
Focusing specifically on the community care field, Modernising Community Care: An Action Plan was published in 1998, five years after the implementation of the relevant sections of the NHS and Community Care Act 1990. The theme of partnership working permeates the Plan: ‘the effectiveness of community care relies on the ability of these organisations to work together and with others to plan and deliver the services people want.’ It should be noted that the then Scottish Homes was considered a key member of the triad. There was concern to make best use of the ‘community care pound’ and to avoid cost shunting between agencies. By the end of 1999 it was felt that the ambition of Modernising Community Care had not been sufficiently progressed and the Joint Future Group was established as a short-life working group by the Minister for Health and Community Care. It reported a year later in Community Care: A Joint Future. Key recommendations were designed to deliver a ‘step-change’, including local partnership agreements; sharing resources, management and information; joint planning frameworks; accelerated take-up of good practice; and all agencies accountable for performance. A number of initiatives were promoted at this time, including rapid response teams in every locality; development of intensive home support/augmented home care schemes; services designed to provide practical support with shopping, domestic and household maintenance tasks; and an annual allocation of £10m to tackle delayed discharge. The Joint Future Unit was formed at this time to progress the Joint Future Agenda; the profile of housing however had faded.
The Community Care and Health (Scotland) Act 2002 introduced legislation that enabled payments between the NHS and local authorities for certain functions of the other agency and allowed for the development of lead commissioning and for pooled (or aligned) budgets.
At the same time the Joint Future Agenda was being pursued through a number of key developments, including Single Shared Assessment, Local Partnership Agreements, and the Joint Performance Information and Assessment Framework.
Over the last six or seven years there has been a shift in focus from the process of partnership working to the delivery of outcomes, embracing both individual outcomes and organisational outcomes. The Joint Improvement Team was established in 2004 and has increasingly focused on achieving better outcomes for people who access support and their carers. Members of the Joint Improvement Team have been at the forefront of progressing the implementation of the Talking Points: Personal Outcomes Approach.
In December 2011 the then Health Secretary, Nicola Sturgeon, made a statement on the future plans for integrated working across health and social care in Scotland. Following a period of engagement with key stakeholders, the proposal set out that the existing Community Health Partnerships will be replaced by Health and Social Care Partnerships. These will be the joint responsibility of the NHS and local authority in each area and will work in partnership with the third and independent sectors. NHS Boards and local authorities will be required to produce integrated budgets for adult services in order to end ‘cost shunting’ across organisations and a jointly accountable officer will be responsible for delivery on this budget. A set of national outcomes will be agreed that all partnerships will be required to deliver. The government had heeded the evidence base and was:
‘keen to avoid the pitfalls that can accompany centrally directed, large-scale structural reorganisation and staff transfer. Evidence from elsewhere is that changes in structures and staffing arrangements work best when designed and agreed locally, to suit the needs of local patients, service users and carers’.
The importance of a focus on personal outcomes and on the local context was emphasised:
‘our approach has started with the key questions about what matters most to people who use these services – what are the improvements they want to see and what are the barriers in the current system that prevent staff from using their skills and resources to best effect’.
The new arrangements will require legislation and guidance and are not expected to be fully implemented before 2015. Underpinning the proposals is the core objective that a shift in the balance of care is achieved such that a smaller proportion of resources (both money and staff) is directed towards institutional care and a greater proportion in vested in community provision.
National Health and Wellbeing Outcomes
-
Healthier Living
People are able to look after and improve their own health and wellbeing and live in good health for longer.
-
Independent Living
People, including those with disabilities or long term conditions, or who are frail, are able to live, as far as reasonably practicable, independently and at home or in a homely setting in their community.
-
Positive Experience
People who use health and social care services have positive experiences of those services, and have their dignity respected.
-
Quality of Life
Health and social care services are centred on helping to maintain or improve the quality of life of people who use those services.
-
Addressing Health Inequalities
Health and social care services contribute to reducing health inequalities.
-
Carers are Supported
People who provide unpaid care are supported to look after their own health and wellbeing, including to reduce any negative impact of their caring role on their own health and well-being.
-
Services are Safe
People who use health and social care services are safe from harm.
-
Engaged Workforce
People who work in health and social care services feel engaged with the work they do and are supported to continuously improve the information, support, care and treatment they provide.
-
Effective Resource Use
Resources are used effectively and efficiently in the provision of health and social care services.
It is important to note that the 2010 NHS Confederation/ADASS survey cited earlier revealed that the top factors that promoted effective integrated working were locally determined; those that inhibited were at the national level. These findings are summarised below:
Help
- Friendly relationships
- Good leadership
- Commitment from the top
- Joint strategy and vision
- Co-terminosity
Hinder
- Performance regimes
- Financial pressures
- Organisational complexity
- Changing leadership
- Financial complexity
A individual level
Learning outcomes
- Identifying the barriers and drivers to integrated working
Time
- Around 45-60 minutes
Materials
- Post-its, flip chart, [table below]
Guidance
Each individual to draw the outlines of two people side by side, but with sufficient space to write between them. The individual is one of the outlines and the other should be a person from a different professional background that they work with. Think about the things that help you to work together and write them between the two outlines. Think about the things that get in the way of the two of you working together and write them in a different colour round the outside. As a group pool your ideas and draw up a composite diagram highlighting the barriers and drivers to working together at the individual level.
Step two - at an organisational level
Repeat the exercise as above, but this time think in terms of two organisations working together eg health and housing, social care and a major provider, a housing association and a mental health team.
Step three - problem solving
Each group to select two of the barriers to integrated working and to outline ways in which they can overcome.
The following matrix is from a study by Stewart et al (2003) of the drivers and barriers to integrated working. A more detailed version can be found at Appendix two.
| Drivers | Barriers | |
|---|---|---|
National policy frameworks |
joined up strategic realistic |
Piecemeal and contradictory Promote ‘projectitis’ Unrealistic change agenda |
Local planning context |
Planning and decision cycles mesh Joint acceptance of unmet need Agreed, comprehensive vision, owned at all levels |
Incompatible planning and decision cycles Not needs led Issues seen in isolation |
Operational factors |
|
|
| Relations between partners |
Trust permits risk-taking Open, honest communication |
Lack of trust prevents risk taking Defensive, limited communication Sees institutional and legal barriers Senior figures devalue/disown Common purpose Presses on regardless Unclear responsibilities, conflict Staff expendable Tribal, protectionist Covers own back ‘We have everything to lose’ ‘No way’ Only seen from agencies’ agenda Invisible Winners and losers |
| Organisational culture |
Can-do culture Collective responsibility publicly demonstrated |
|
| Change management | Flexible enough to learn as goes | |
| Enabling staff |
Agreed roles and responsibilities Staff valued |
|
| Professional behaviour |
Centred on user need Willing to take risks |
|
| Attitudes |
‘We have nothing to lose’ ‘We will find a way’ |
|
| Outcomes |
User focused Visible Benefits shared |
An alternative formulation is presented in diagrammatic form below.

Source: Jelphs and Dickinson (2008)
Learning outcomes
- Identifying the roles of different professionals in integrated working
- aluing the unique roles of different professionals
- Identifying where there are opportunities to share common roles
Time
- No more than 30 minutes
Materials
- Post-its, flip chart
Guidance
- Divide into small mixed groups. Each individual to think of their own role and identify the tasks they do that they think can only be done by their profession and what is/can be generic with other professions. Write each of these different tasks on post-its. There may be some discussion here of what has traditionally been done by one profession but may not necessarily be a requirement going forward. It may also be useful to think of the individual’s journey and the various support that may be required.
- Draw overlapping circles on a flip chart sheet, one circle for each profession in the group.
- Individuals to read out their post-its and then add to the relevant part of the flip chart – in the overlapping section if shared tasks, in the section unique to their profession if seen as unique.
- Group similar features and discuss the similarities and differences that are emerging and whether there are roles agreed as distinct to each profession and roles considered more generic.